Sedation
471 - Bispectral Index System Assessment of a Propofol Infusion Kinetic-Based Program

Ayah Koleilat, DDS
Resident
University at Buffalo/Women and Children’s Hospital of Buffalo, Buffalo, NY
University at Buffalo School of Dental Medicine
Amherst, New York, United States
Brigid Daly, DDS
PGY-2
University at Buffalo/Women and Children’s Hospital of Buffalo, Buffalo, NY
University at Buffalo
BUFFALO, New York, United States- AL
Allana Langen, Bachelor's of Science, Sociology and English
University Pediatric Dentistry
- JM
Jonathan Malinovsky, BS
University Pediatric Dentistry

Christopher Heard, MD
Attending Anesthesiologist
University at Buffalo
Buffalo, New York, United States
Christopher Heard, MD
Attending Anesthesiologist
University at Buffalo
Buffalo, New York, United States- CW
Carrie Wanamaker, DDS, DDS
Program Director, Advanced Education in Pediatric Dentistry
University at Buffalo
Buffalo, New York, United States
Presenting Author(s)
Co-Author(s)
Research Mentor(s)
Program Director(s)
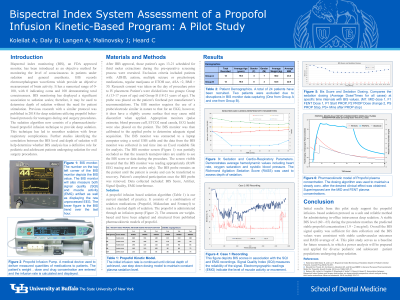
Purpose: This research investigates the Bispectral Index System (BIS) scores of patients undergoing dental procedures using a propofol infusion-based intravenous sedation algorithm.
Methods: After Institutional Review Board approval, patients aged 13 to 21 years who reported for third-molar extractions were recruited. The BIS probe was placed on the participant’s forehead during their procedure. During treatment, raw data was gathered in real time from the BIS monitor via a laptop; study staff were blinded to the scores as this occurred. Patient demographics, health history, and procedural details were collected from the patient’s sedation record. Descriptive statistics were used to define the results.
Results: To date, 8 patients have been recruited; one patient was excluded from analysis. The average airway score was 6.0, denoting the necessity for supplemental oxygen and chin lift. The mean Richmond Agitation-Sedation Score was -4, the desired depth of sedation. BIS scores from the initiation of the sedation ranged from 96.6 to 97.7. Scores fluctuated mildly throughout the procedures. The lowest scores ranged from 24.6 to 45.8. The BIS monitor’s signal quality ranged from 75.3 to 84.3.
Conclusion: BIS quality signal was continuously over 50, indicating sufficient quality for data gathering. Initial results support the BIS monitor as an effective tool for assessing depth and quality of sedation. Data collection will continue until 48 patients are analyzed. We anticipate that completion of data collection will allow us to prepare a power analysis for future research.

.png)