CMR-Analysis (including machine learning)
1357635 - Multi-modal comparison of aorta morphology in patients with aortopathy: 3D mDixon CMR versus 4D Flow MRI versus Computed Tomographic angiography.
- FG
Faeze Gholamiankhah, MSc
Ph.D. Candidate
Leiden University Medical Center
Maarssen, Netherlands - FG
Faeze Gholamiankhah, MSc
Ph.D. Candidate
Leiden University Medical Center
Maarssen, Netherlands 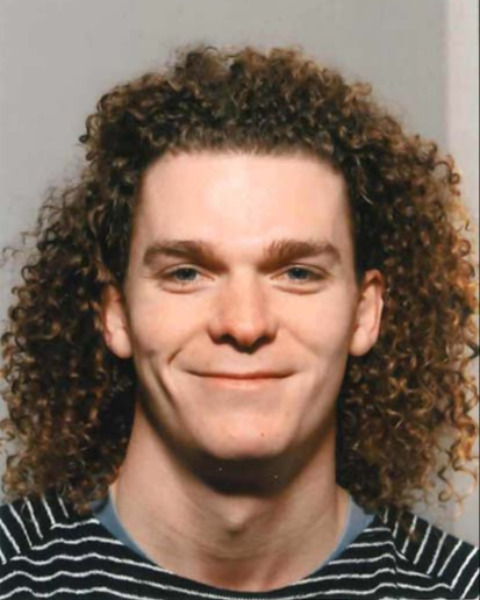
Joe f. Juffermans, MSc
PhD Candidate
Leiden University Medical Center
Leiden, Zuid-Holland, Netherlands- Bt
Bastiaan J.C. te Kiefte, MD
Radiology Resident & PhD Candidate
Leiden University Medical Center, Netherlands - Pv
Pieter van den Boogaard, BSc
Sr. radiodiagnostic technologist
Leiden University Medical Center, Zuid-Holland, Netherlands 
Jos J.M. Westenberg, PhD
Associate Professor
Leiden University Medical Center
Leiden, Zuid-Holland, Netherlands
Hildo Lamb, MD, PhD
Radiology Professor
Leiden University Medical Center
Leiden, Zuid-Holland, Netherlands
Presenting Author(s)
Primary Author(s)
Co-Author(s)
Methods:
This retrospective study included twenty-one subjects (14 men, 7 women, mean age: 51 ± 18). The median [interquartile range] time interval between CMR and CTA was 95 [58, 248] days.
CTA and 3D mDixon images were segmented using ITK-SNAP and 4D flow MRI was segmented at peak systole using CAAS MR Solutions v5.1 (Pie Medical Imaging). Representative examples of images and segmentations are shown in Fig. 1. Maximum diameter, volume, and centerline length were calculated for four segments of each aortic lumen including aortic root, ascending aorta, aortic arch, and thoracic descending aorta. The measurements were analysed using Pearson correlation, independent samples T-test and Bland-Altman plots.
Results: The statistics of measurements are summarized in table 1. The reported P-values are greater than 0.05 for all parameters across each aortic level, demonstrating that there is no significant difference between paired values of 4D flow, mDixon and CTA images. Maximum aortic diameter showed very strong correlation between all modalities (correlation coefficient > 0.85). Also, measurements of volume and centerline length were strongly correlated between mDixon and CTA. However, comparison of 4D flow MRI and CTA outcomes revealed less correlation in terms of volume and centerline length in aortic root segment. Bland-Altman analysis as illustrated in fig. 2 showed a higher limit of agreement between CTA and 4D flow data compared to CTA and mDixon data, especially in volume measurements (27.6 vs. 20.4 mL). Moreover, underestimation in values of 4D flow MRI and overestimation in values of mDixon were observed when compared with CTA.
Conclusion: Maximum diameter assessment in the thoracic aorta in patients with aortopathy shows strong agreement between 3D mDixon CMR, 4D flow MRI, and CTA. Aortic volume and centerline length assessment are also in strong agreement between modalities, except for 4D flow MRI in the aortic root. During follow-up imaging, patients could be subjected to various modalities and sequences, and this study demonstrates the comparability of outcomes.
