Back
Introduction: To assess urologists’ attitudes toward treating LGBT patients and counseling practices during diagnosis and treatment of prostate cancer (PCa)
Methods: A 35-question, 3-part (history taking, health training, and PCa counseling) survey was sent to program directors of U.S. urology residencies. Demographics were also collected
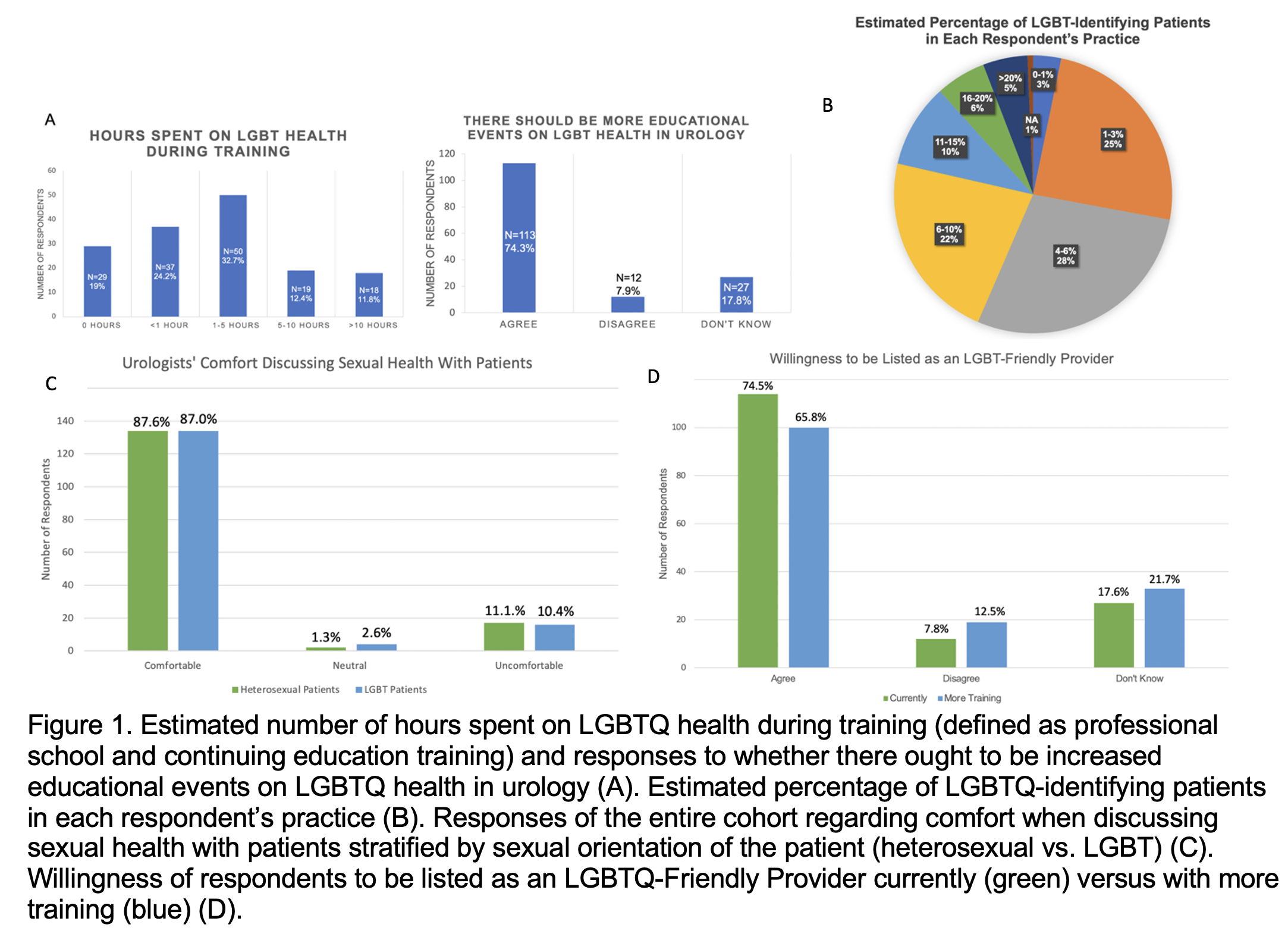
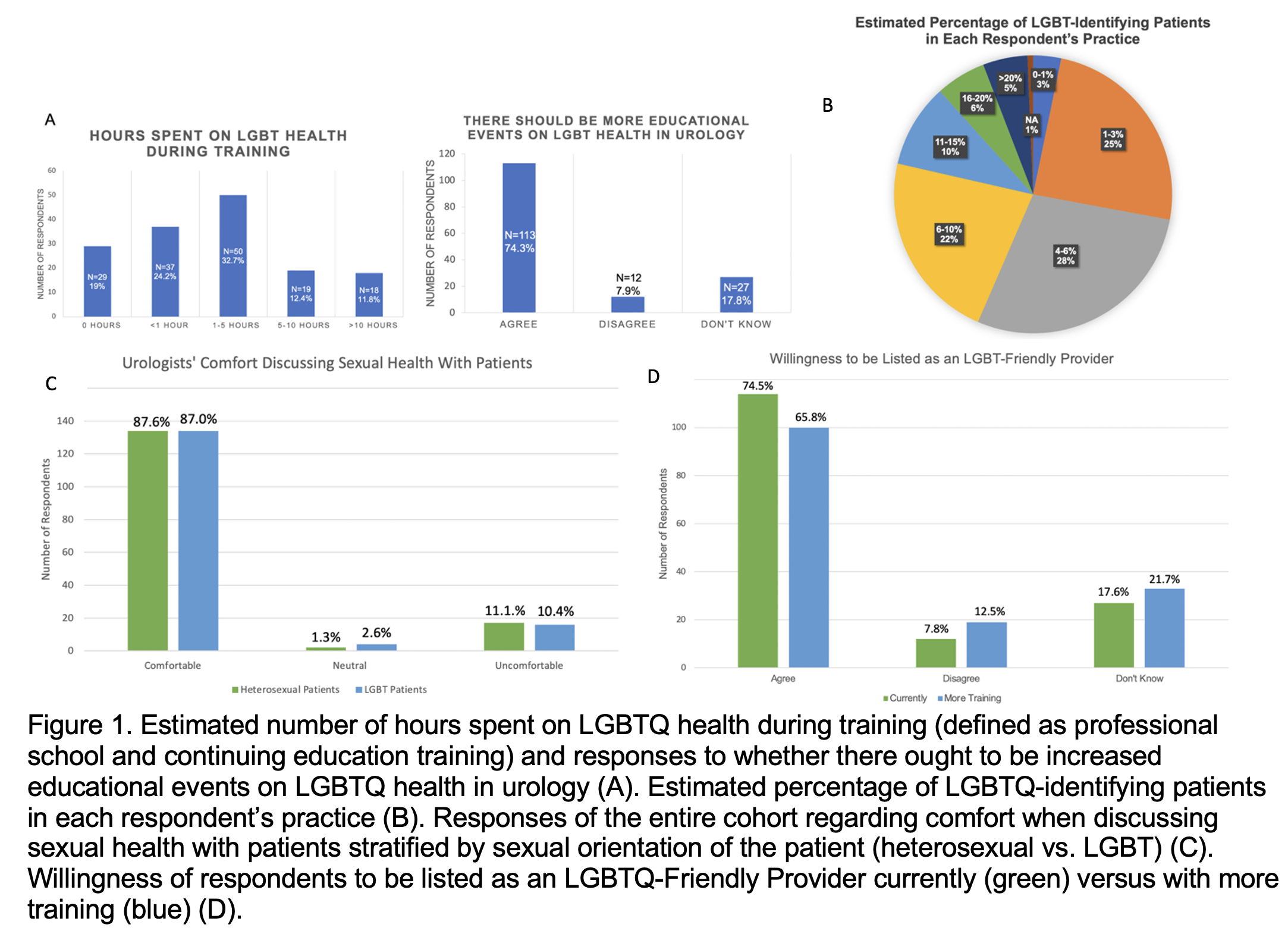
Results: 154 responses met inclusion criteria. Compared to the 2021 AUA Census, our cohort skewed younger and included a higher proportion of academic, female and gay-identifying providers. 54.2% of respondents don’t assume patients are heterosexual. While 87% feel comfortable discussing sexual health with LGBTQ patients, 42.9% disagree that knowing sexual orientation is necessary to providing optimal care. Physicians >65 years old are more likely to believe that knowing sexual orientation is necessary to provide the best care (p=0.034) but younger and academic physicians are more likely to elicit this during history taking (p=0.037, p=0.007) and via intake forms (p=0.009, p=0.002). A majority (32.7%) report 1-5 hours of LGBTQ health training. 74.3% believe more training is needed. 74.5% would agree to being listed as an LGBTQ-Friendly Provider currently, 65.8% would want additional training. Female (p=0.01) and younger providers (p=0.038) are more likely to request more training. Younger providers believe more strongly in additional educational events (p=0.009). North Central and South Central AUA sections are most likely to have 0 hours of LGBTQ education in medical school and Western and Northeastern sections are most likely to have >10 hours (p=0.012). 63.6% agree the prostate is a source of sexual pleasure. 55.9% believe it important to assess sexual satisfaction in patients who engage in receptive anal intercourse after PCa treatment. Responses were mixed on timing of receptive anal intercourse after treatment and counseling on anal stimulation prior to PSA testing. Answers to knowledge questions on anal cancer and communication were primarily correct; answers to questions on anejaculation and health care differences were mixed.
Conclusions: Education is necessary on specific differences between heterosexual and LGBTQ patient concerns and application of this knowledge to address the needs of an aging LGBTQ population SOURCE OF
Funding: NA
Moderated Poster Session
Session: MP21: Diversity, Equity & Inclusion: Health Equity & Outcomes II
MP21-01: Urologists and LGBTQ Patients: A qualitative study of the practice patterns, attitudes, and knowledge base of urologists toward their LGBTQ Patients
Friday, April 28, 2023
3:30 PM – 5:30 PM CST
Location: S404C
- AX
Poster Presenter(s)
Introduction: To assess urologists’ attitudes toward treating LGBT patients and counseling practices during diagnosis and treatment of prostate cancer (PCa)
Methods: A 35-question, 3-part (history taking, health training, and PCa counseling) survey was sent to program directors of U.S. urology residencies. Demographics were also collected
Results: 154 responses met inclusion criteria. Compared to the 2021 AUA Census, our cohort skewed younger and included a higher proportion of academic, female and gay-identifying providers. 54.2% of respondents don’t assume patients are heterosexual. While 87% feel comfortable discussing sexual health with LGBTQ patients, 42.9% disagree that knowing sexual orientation is necessary to providing optimal care. Physicians >65 years old are more likely to believe that knowing sexual orientation is necessary to provide the best care (p=0.034) but younger and academic physicians are more likely to elicit this during history taking (p=0.037, p=0.007) and via intake forms (p=0.009, p=0.002). A majority (32.7%) report 1-5 hours of LGBTQ health training. 74.3% believe more training is needed. 74.5% would agree to being listed as an LGBTQ-Friendly Provider currently, 65.8% would want additional training. Female (p=0.01) and younger providers (p=0.038) are more likely to request more training. Younger providers believe more strongly in additional educational events (p=0.009). North Central and South Central AUA sections are most likely to have 0 hours of LGBTQ education in medical school and Western and Northeastern sections are most likely to have >10 hours (p=0.012). 63.6% agree the prostate is a source of sexual pleasure. 55.9% believe it important to assess sexual satisfaction in patients who engage in receptive anal intercourse after PCa treatment. Responses were mixed on timing of receptive anal intercourse after treatment and counseling on anal stimulation prior to PSA testing. Answers to knowledge questions on anal cancer and communication were primarily correct; answers to questions on anejaculation and health care differences were mixed.
Conclusions: Education is necessary on specific differences between heterosexual and LGBTQ patient concerns and application of this knowledge to address the needs of an aging LGBTQ population SOURCE OF
Funding: NA