Back
Introduction: The use of synthetic mesh in the treatment of pelvic floor conditions has long been scrutinized. Statements from multiple professional societies recommend that mesh for pelvic organ prolapse (POP) be performed only by those properly trained in both implantation and management of complications. We used case logs from the American Board of Urology (ABU) to understand temporal changes in the use of pelvic mesh among subspecialty trained and general urologists.
Methods: Case logs submitted to the ABU for certification and recertification in 2013 and in 2020 were reviewed. Demographic data including surgeon age, fellowship training, certification cycle, and practice type and location was analyzed. We analyzed trends in mesh insertion (both for POP and SUI) and mesh revision/removal based using common procedural terminology (CPT) codes among FPMRS and general urologists. Statistical analysis was performed using chi-squared test, binary regression, and Cronbach’s alpha.
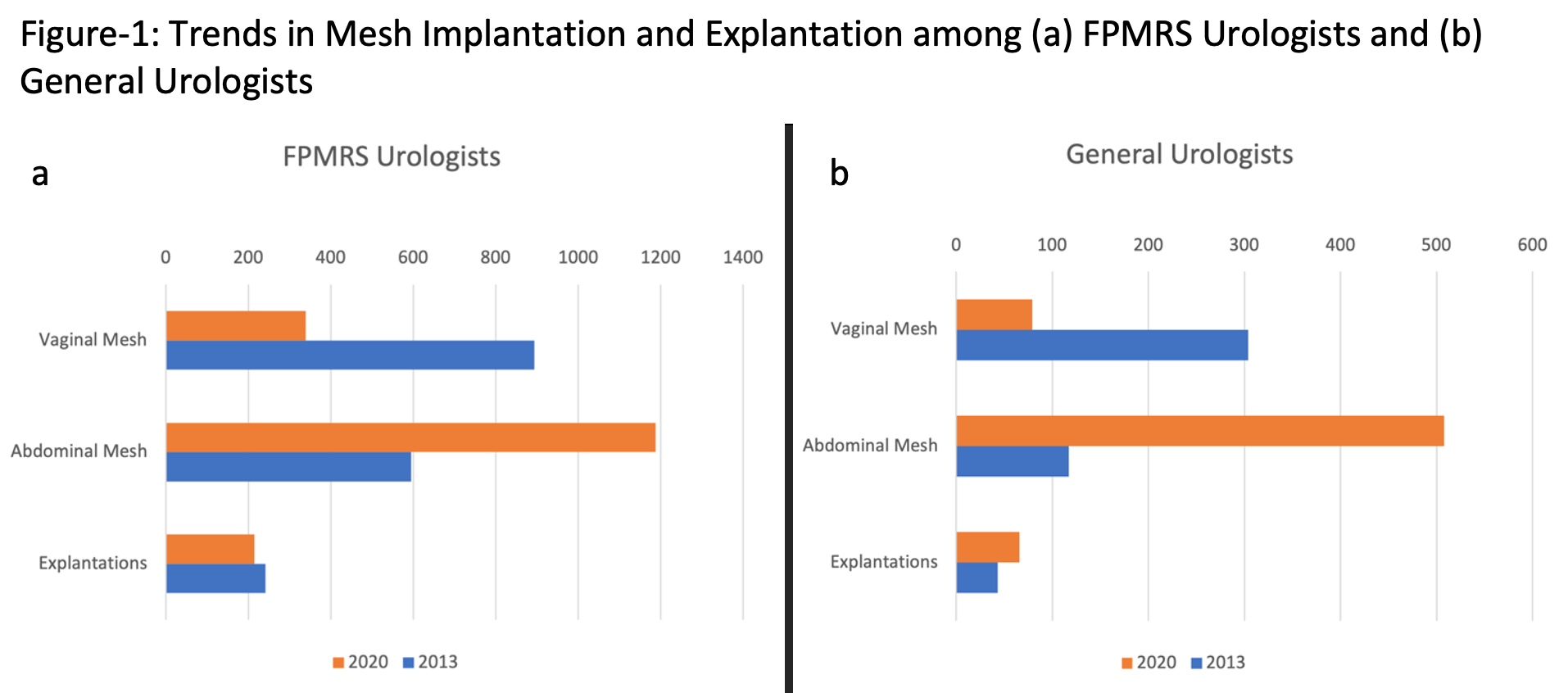
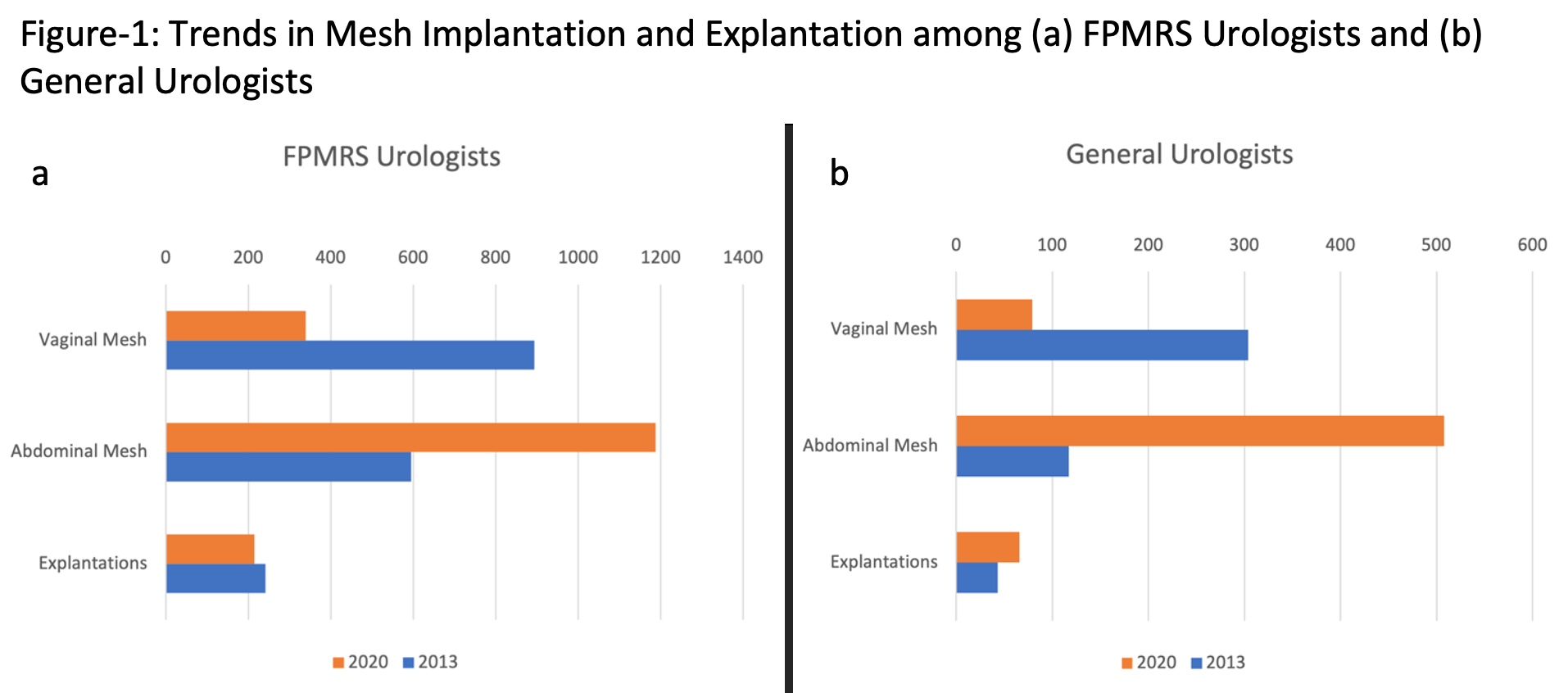
Results: Over the two study years, 1877 surgeons contributed 253,326 unique procedures. A total of 1910 (1.8% of total cases) mesh implantation procedures were performed in 2013 compared to 2245 (1.5%) in 2020. Among FPMRS providers (n=154, 8.2%), the use of vaginal mesh for POP decreased from 4.6% to 1.5% (p <.001) of their total procedure volume, while transabdominal mesh for POP increased from 3.1% to 5.3%, (p <.001, see Figure-1). Similar changes were seen among generalists, among whom the rate tripled (0.1% to 0.4%, p<.001, see Figure-1b). Mesh revision/removal rates were stable (2.9%, p=.224) among FPMRS providers, but significantly decreased among general urologists in 2020 (0.2% to 0.1% p<.001). On multivariable analysis, generalists more likely to perform mesh revisions/removals were non-academic, female, and practiced in areas with a population density = 1 million. Generalists implanting mesh were also more likely to perform revision/removal (Cronbach’s alpha = 0.343, p=.015).
Conclusions: Mesh-augmented POP repairs continue to be used among FPMRS and general urologists. However, these data indicate that general urologists may be referring mesh complications onto FPMRS providers, indicating that societal and FDA recommendations are perhaps not being adhered to. SOURCE OF
Funding: The Catherine and Joseph Aresty Department of Urology
Moderated Poster Session
Session: MP07: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Pelvic Prolapse
MP07-09: Trends in Implantation and Explantation of Mesh for Pelvic Organ Prolapse among FPMRS and General Urologists
Friday, April 28, 2023
9:30 AM – 11:30 AM CST
Location: S401A

Mitchell G. Goldenberg, MD
University of Southern California
Poster Presenter(s)
Introduction: The use of synthetic mesh in the treatment of pelvic floor conditions has long been scrutinized. Statements from multiple professional societies recommend that mesh for pelvic organ prolapse (POP) be performed only by those properly trained in both implantation and management of complications. We used case logs from the American Board of Urology (ABU) to understand temporal changes in the use of pelvic mesh among subspecialty trained and general urologists.
Methods: Case logs submitted to the ABU for certification and recertification in 2013 and in 2020 were reviewed. Demographic data including surgeon age, fellowship training, certification cycle, and practice type and location was analyzed. We analyzed trends in mesh insertion (both for POP and SUI) and mesh revision/removal based using common procedural terminology (CPT) codes among FPMRS and general urologists. Statistical analysis was performed using chi-squared test, binary regression, and Cronbach’s alpha.
Results: Over the two study years, 1877 surgeons contributed 253,326 unique procedures. A total of 1910 (1.8% of total cases) mesh implantation procedures were performed in 2013 compared to 2245 (1.5%) in 2020. Among FPMRS providers (n=154, 8.2%), the use of vaginal mesh for POP decreased from 4.6% to 1.5% (p <.001) of their total procedure volume, while transabdominal mesh for POP increased from 3.1% to 5.3%, (p <.001, see Figure-1). Similar changes were seen among generalists, among whom the rate tripled (0.1% to 0.4%, p<.001, see Figure-1b). Mesh revision/removal rates were stable (2.9%, p=.224) among FPMRS providers, but significantly decreased among general urologists in 2020 (0.2% to 0.1% p<.001). On multivariable analysis, generalists more likely to perform mesh revisions/removals were non-academic, female, and practiced in areas with a population density = 1 million. Generalists implanting mesh were also more likely to perform revision/removal (Cronbach’s alpha = 0.343, p=.015).
Conclusions: Mesh-augmented POP repairs continue to be used among FPMRS and general urologists. However, these data indicate that general urologists may be referring mesh complications onto FPMRS providers, indicating that societal and FDA recommendations are perhaps not being adhered to. SOURCE OF
Funding: The Catherine and Joseph Aresty Department of Urology