Back
Introduction: As surgical training has become increasingly subspecialized, residents have been encouraged to pursue additional fellowship training. We sought to better understand current attitudes regarding expectations for competency for non-fellowship trained graduates in sub-specialty procedures and how this has affected teaching practices during residency training. We chose to study hypospadias as a model as it is a signature procedure for pediatric urologists that is both technically challenging and at the same time quite common.
Methods: We created a survey tool utilizing the well-established Zwisch scale to assess the level of autonomy afforded to trainees by survey respondents during various types of hypospadias repair as well as elicited attitudes regarding post-training expectations. Our survey was distributed via email to the Society of Pediatric Urology membership. We also collected respondent demographic data such as geographic location, years in practice, and practice setting.
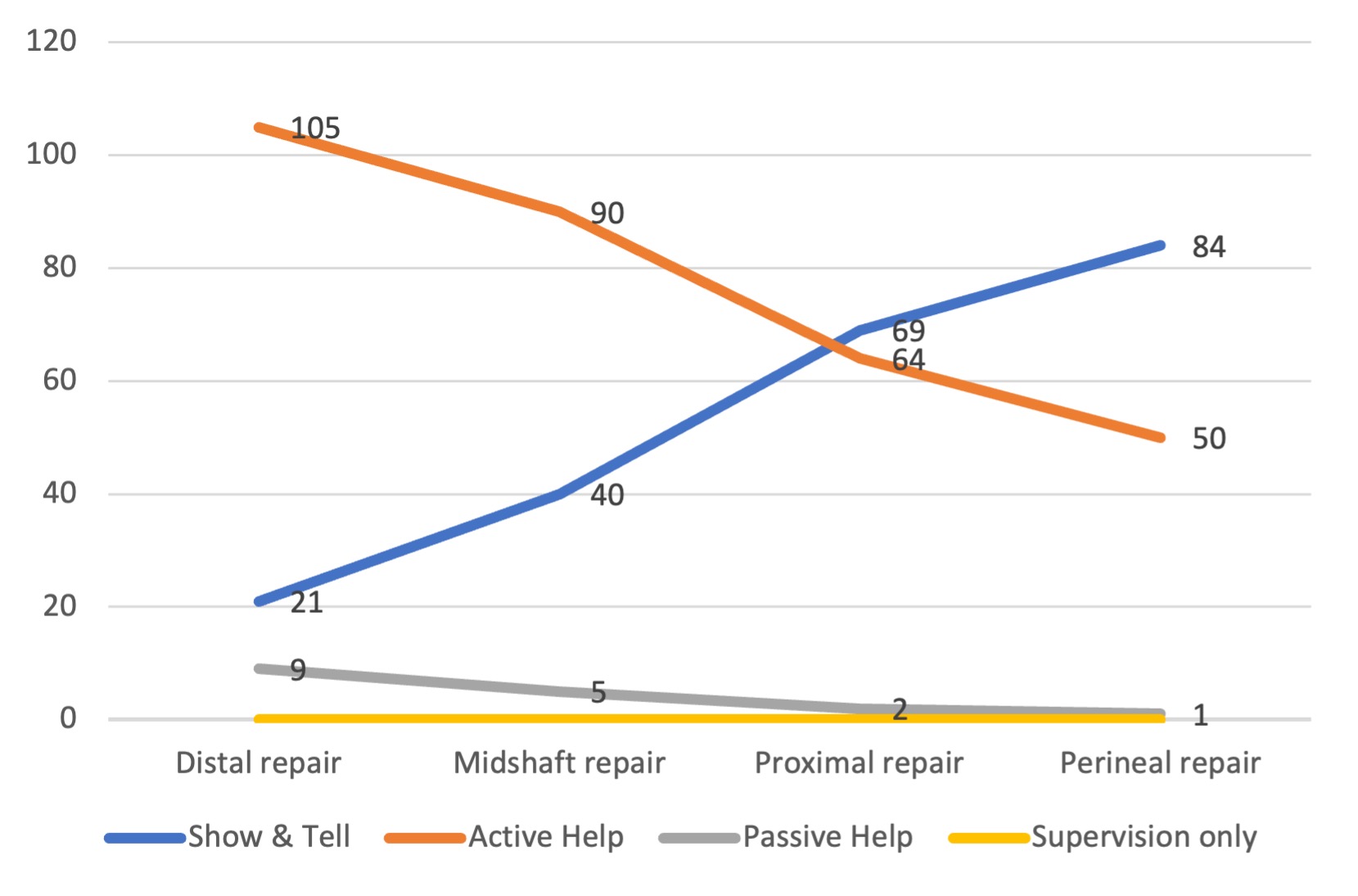
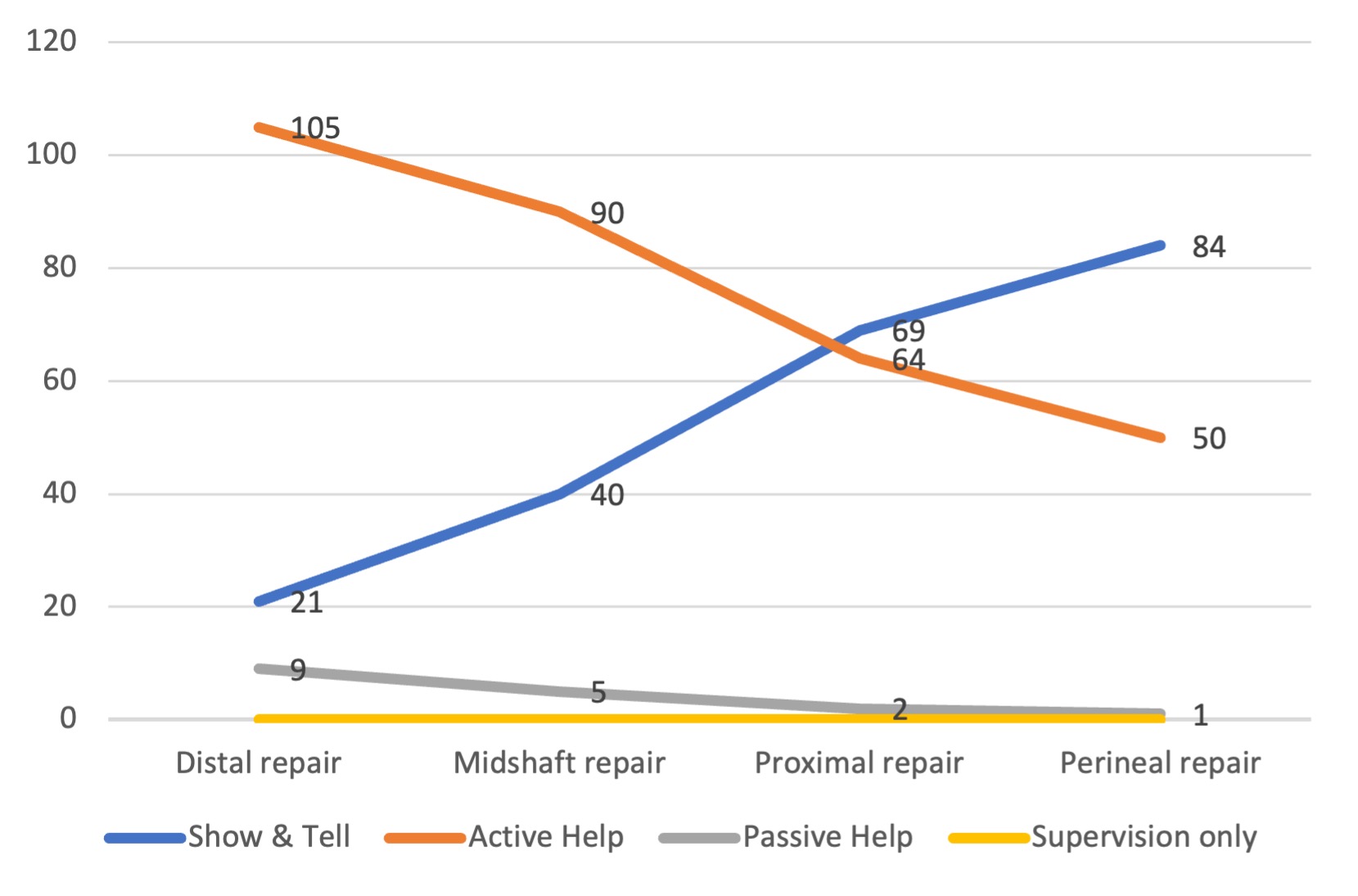
Results: 178 of 761 (23%) unique recipients completed the survey. We excluded 6 respondents who are retired or do not perform hypospadias repair. 170 of 172 (98%) included respondents felt that trainees should not perform hypospadias repair independently in practice without additional fellowship training. Among pediatric urologists who train residents, trainee autonomy as measured by the Zwisch scale was limited to an assistant role for the vast majority of trainees and decreased as the severity of the hypospadias increased (Figure 1).
Conclusions: Urology residents for the most part are not being afforded a level of autonomy in hypospadias cases during training that would suggest competency for independence following graduation. Additionally, there is consensus that contemporary graduates are not expected to be competent to perform hypospadias repair in independent practice without additional fellowship training. This raises the question if there are other common sub-specialty procedures in urology where residents are not expected to achieve competence, and if so, how should we as educators, be forthcoming about the limitations of urology residency training to set appropriate trainee and employer expectations? SOURCE OF
Funding: None.
Moderated Poster Session
Session: MP18: Pediatrics II
MP18-08: Should contemporary urology residents expect to be able perform hypospadias repair when they graduate without fellowship training: results from a survey of SPU membership.
Friday, April 28, 2023
1:00 PM – 3:00 PM CST
Location: S505

Aurash NaserTavakolian, MD (he/him/his)
Cedars-Sinai Medical Center
Poster Presenter(s)
Introduction: As surgical training has become increasingly subspecialized, residents have been encouraged to pursue additional fellowship training. We sought to better understand current attitudes regarding expectations for competency for non-fellowship trained graduates in sub-specialty procedures and how this has affected teaching practices during residency training. We chose to study hypospadias as a model as it is a signature procedure for pediatric urologists that is both technically challenging and at the same time quite common.
Methods: We created a survey tool utilizing the well-established Zwisch scale to assess the level of autonomy afforded to trainees by survey respondents during various types of hypospadias repair as well as elicited attitudes regarding post-training expectations. Our survey was distributed via email to the Society of Pediatric Urology membership. We also collected respondent demographic data such as geographic location, years in practice, and practice setting.
Results: 178 of 761 (23%) unique recipients completed the survey. We excluded 6 respondents who are retired or do not perform hypospadias repair. 170 of 172 (98%) included respondents felt that trainees should not perform hypospadias repair independently in practice without additional fellowship training. Among pediatric urologists who train residents, trainee autonomy as measured by the Zwisch scale was limited to an assistant role for the vast majority of trainees and decreased as the severity of the hypospadias increased (Figure 1).
Conclusions: Urology residents for the most part are not being afforded a level of autonomy in hypospadias cases during training that would suggest competency for independence following graduation. Additionally, there is consensus that contemporary graduates are not expected to be competent to perform hypospadias repair in independent practice without additional fellowship training. This raises the question if there are other common sub-specialty procedures in urology where residents are not expected to achieve competence, and if so, how should we as educators, be forthcoming about the limitations of urology residency training to set appropriate trainee and employer expectations? SOURCE OF
Funding: None.