Back

Poster Session D - Tuesday Morning
Category: Esophagus
D0250 - A Case of Esophageal Intramural Pseudodiverticulosis
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
Sarah Arvaneh, DO
Larkin Community Hospital
Doral, FL
Presenting Author(s)
Sarah Arvaneh, DO1, Jonathan Mendoza, DO2, Karthik Mohan, DO3
1Larkin Community Hospital, Doral, FL; 2Larkin Community Hospital, Hialeah, FL; 3Palmetto General Hospital, Hialeah, FL
Introduction: Esophageal intramural pseudodiverticulosis (EIP) is a rare benign condition, presenting in < 1%
of endoscopy cases. It’s trademark appearance is that of a flask-shaped outpouching lesions
along the esophageal wall. It is known to coexist with gastroesophageal reflux disease (GERD),
esophageal stricture, diabetes, alcohol dependence syndrome, and achalasia. They are not
considered true diverticula due to them morphologically consisting of widened secretory ducts of
the submucosal glands. Patients with EIP present most commonly complaining of dysphagia.
Patients generally are diagnosed by barium swallow study, computed tomography, and
endoscopy; with endoscopic ultrasound being used for further determination of the layers
involved.
Here we present a case of a patient with a previously treated esophageal stricture who suffered
from chest pain and was diagnosed with EIP by esophago-gastro-duodenoscopy (EGD).
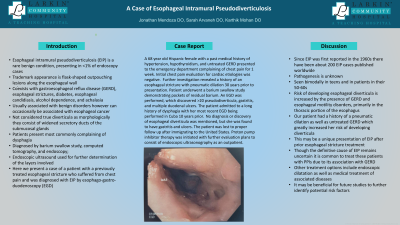
Case Description/Methods: A 68 year old Hispanic female with a history of hypertension, hypothyroidism, and untreated
GERD presented to the emergency department complaining of chest pain for 1 week. Initial
chest pain evaluation for cardiac results were negative, further investigation revealed a history of
esophageal stricture with pneumatic dilation 30 years prior to presentation. Patient underwent a
barium swallow study demonstrating pockets of residual barium. An EGD was performed,
discovering >20 pseudodiverticula, gastritis, and multiple duodenal ulcers. The patient admitted
to a long history of dysphagia with her most recent EGD being performed in Cuba 10 years prior.
No diagnosis or discovery of esophageal diverticula was mentioned, but was found to have
gastritis and ulcers at that time. Proton pump inhibitor therapy was initiated with further evaluation plans to consist of
endoscopic ultrasonography.
Discussion: The risk of developing esophageal diverticula is increased by the presence of GERD and
esophageal motility disorder, primarily in the thoracic portion of the esophagus. In this case, our
patient had a history of a pneumatic dilation as well as untreated GERD which greatly increased
her risk of developing diverticula. This may be a unique presentation of EIPD after prior
esophageal stricture treatment. Though the definitive cause of EIPD remains uncertain at this
time, it is common to treat these patients with PPIs due to its association with GERD. It may be
beneficial for future studies to further identify potential high risk factors.
Disclosures:
Sarah Arvaneh, DO1, Jonathan Mendoza, DO2, Karthik Mohan, DO3. D0250 - A Case of Esophageal Intramural Pseudodiverticulosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Larkin Community Hospital, Doral, FL; 2Larkin Community Hospital, Hialeah, FL; 3Palmetto General Hospital, Hialeah, FL
Introduction: Esophageal intramural pseudodiverticulosis (EIP) is a rare benign condition, presenting in < 1%
of endoscopy cases. It’s trademark appearance is that of a flask-shaped outpouching lesions
along the esophageal wall. It is known to coexist with gastroesophageal reflux disease (GERD),
esophageal stricture, diabetes, alcohol dependence syndrome, and achalasia. They are not
considered true diverticula due to them morphologically consisting of widened secretory ducts of
the submucosal glands. Patients with EIP present most commonly complaining of dysphagia.
Patients generally are diagnosed by barium swallow study, computed tomography, and
endoscopy; with endoscopic ultrasound being used for further determination of the layers
involved.
Here we present a case of a patient with a previously treated esophageal stricture who suffered
from chest pain and was diagnosed with EIP by esophago-gastro-duodenoscopy (EGD).
Case Description/Methods: A 68 year old Hispanic female with a history of hypertension, hypothyroidism, and untreated
GERD presented to the emergency department complaining of chest pain for 1 week. Initial
chest pain evaluation for cardiac results were negative, further investigation revealed a history of
esophageal stricture with pneumatic dilation 30 years prior to presentation. Patient underwent a
barium swallow study demonstrating pockets of residual barium. An EGD was performed,
discovering >20 pseudodiverticula, gastritis, and multiple duodenal ulcers. The patient admitted
to a long history of dysphagia with her most recent EGD being performed in Cuba 10 years prior.
No diagnosis or discovery of esophageal diverticula was mentioned, but was found to have
gastritis and ulcers at that time. Proton pump inhibitor therapy was initiated with further evaluation plans to consist of
endoscopic ultrasonography.
Discussion: The risk of developing esophageal diverticula is increased by the presence of GERD and
esophageal motility disorder, primarily in the thoracic portion of the esophagus. In this case, our
patient had a history of a pneumatic dilation as well as untreated GERD which greatly increased
her risk of developing diverticula. This may be a unique presentation of EIPD after prior
esophageal stricture treatment. Though the definitive cause of EIPD remains uncertain at this
time, it is common to treat these patients with PPIs due to its association with GERD. It may be
beneficial for future studies to further identify potential high risk factors.
Disclosures:
Sarah Arvaneh indicated no relevant financial relationships.
Jonathan Mendoza indicated no relevant financial relationships.
Karthik Mohan indicated no relevant financial relationships.
Sarah Arvaneh, DO1, Jonathan Mendoza, DO2, Karthik Mohan, DO3. D0250 - A Case of Esophageal Intramural Pseudodiverticulosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
