Sedation
525 - Utilizing Simulation in Resident Sedation Education: Measuring Performance and Self-Efficacy

Marlee Hansen, DDS
Resident
Ohio State University, Columbus, OH
The Ohio State University
Cedar Rapids, Iowa, United States- BM
Beau D. Meyer, DDS, MPH
Assistant Professor
The Ohio State University/Nationwide Children's Hospital
Columbus, Ohio, United States - JT
Janice A. Townsend, DDS, MS
The Ohio State University, Nationwide Children's Hospital
- KH
Kim Hammersmith, DDS, MPH, MS
Program Director
The Ohio State University
Columbus, Ohio, United States - BM
Beau D. Meyer, DDS, MPH
Assistant Professor
The Ohio State University/Nationwide Children's Hospital
Columbus, Ohio, United States 
Daniel Claman, DDS
Associate Program Director
The Ohio State University/Nationwide Children's Hospital
The Ohio State University/Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Co-Author(s)
Research Mentor(s)
Program Director(s)
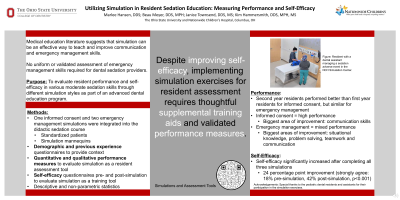
Purpose: To evaluate resident performance and self-efficacy in various moderate sedation skills through different simulation styles as part of an advanced dental education program.
Methods: Simulation exercises for informed consent via standardized patients and emergency management via mannequins were integrated into the resident sedation curriculum. Resident performance was evaluated quantitatively by a standardized form completed by an attending faculty and qualitatively through reflection exercises. Resident self-efficacy was measured via a pre- and post-survey. Descriptive and non-parametric statistics were calculated.
Results: Sixteen residents completed three simulations each. Second year residents tended to perform better than first year residents in both informed consent and emergency simulations; however, the difference was only statistically significant for the informed consent simulation (P < .02). Self-efficacy significantly increased after completing the simulations (18% strongly agreed with self-efficacy statements pre-simulation versus 42% post-simulation, P < .0001). Overall, 61% strongly agreed that the simulations were helpful. The qualitative analysis of reflections revealed that residents felt prepared with the technical elements of informed consent, but not as much for emergency management. Residents identified communication skills as an area of improvement for both simulations. For emergency management, residents felt that more work was needed in knowledge, problem-solving skills, and teamwork.
Conclusions: Simulations were effective at improving self-efficacy in emergency management and informed consent. While self-efficacy increased, residents approaching graduation still felt unprepared in many facets of managing a sedation-related emergency. Simulation training can address these deficits, but best practices in terms of simulation style, frequency, and combination with other education modalities needs clarification.

.png)