Patient Management
143 - Effect of Virtual Reality on Pediatric Dental Patients
.jpg)
Sarah Arafat, MPH, DDS
2nd year Pediatric Resident
University of Texas — Houston, Houston, TX
University of Texas School of Dentistry at Houston
Houston, Texas, United States
Brett T. Chiquet, DDS, PhD
Associate Professor Non-Tenure Clinical
University of Texas Health Science Center at Houston School of Dentistry
University of Texas School of Dentistry
Houston, Texas, United States- JB
Juliana Barros, DDS, MS
Associate Professor & Vice Chair, Department of Restorative Dentistry & Prosthodontics
University of Texas Health Science Center at Houston School of Dentistry
Houston, Texas, United States - GB
Gisela Bona, DDS, MS
The University of Texas School of Dentistry at Houston Pediatric Dental Residency Program
- PR
Priyanshi Ritwik, BDS, MS
Professor
University of Texas Health Science Center at Houston
Houston, Texas, United States - NH
Nathaniel Holland, PhD
UTHealth School of Dentistry
- NS
Nathanael Salako, BDS, MSc
UTHealth School of Dentistry Department of Pediatric Dentistry
- MF
Mary Farach-Carson, PhD
UTHealth School of Dentistry
- SP
Shalizeh Patel, DDS, MEd
UT Health School of Dentistry
Houston, Texas, United States 
Brett T. Chiquet, DDS, PhD
Associate Professor Non-Tenure Clinical
University of Texas Health Science Center at Houston School of Dentistry
University of Texas School of Dentistry
Houston, Texas, United States
Presenting Author(s)
Co-Author(s)
Research Mentor(s)
Program Director(s)
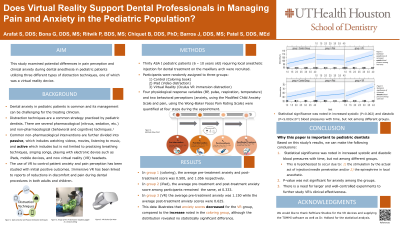
Purpose: This study examined the potential differences in pain perception and clinical anxiety during dental anesthesia in pediatric patients utilizing three different types of distraction techniques, one of which was a virtual reality device.
Methods: Thirty ASA I pediatric patients (6 – 10 years old) requiring local anesthetic injection for dental treatment on the maxillary arch were recruited. The study was approved by the institutional IRB and research consent was obtained from the legal guardian of each patient. Assent from the child was also obtained when applicable. Participants were randomly assigned to three groups: (1) Virtual Reality (Oculus VR for immersion distraction), (2) iPad (video distraction), and (3) control (coloring book). Four physiological response variables (BP, pulse, respiration, temperature) and two behavioral perceptions (anxiety, pain) were quantified at four steps during the treatment appointment.
Results: Statistical significance was noted in increased systolic (P < 0.01) and diastolic (P < 0.00001) blood pressures with time, but not among different groups. P-value was not significant for anxiety. There was a significant effect in pain and time among groups. Pain increased with time in the control and VR groups, but not in the iPad group.
Conclusions: Distraction techniques have the potential to be used for behavior management in pediatric dentistry, and the need for larger, well-controlled study to further investigate VR’s effectiveness must be pursued.

.png)